RICHMOND, Va. (WRIC) -Virginia is transforming its response to mental health crisis calls but some fear underfunding and workforce shortages could hinder the roll out.
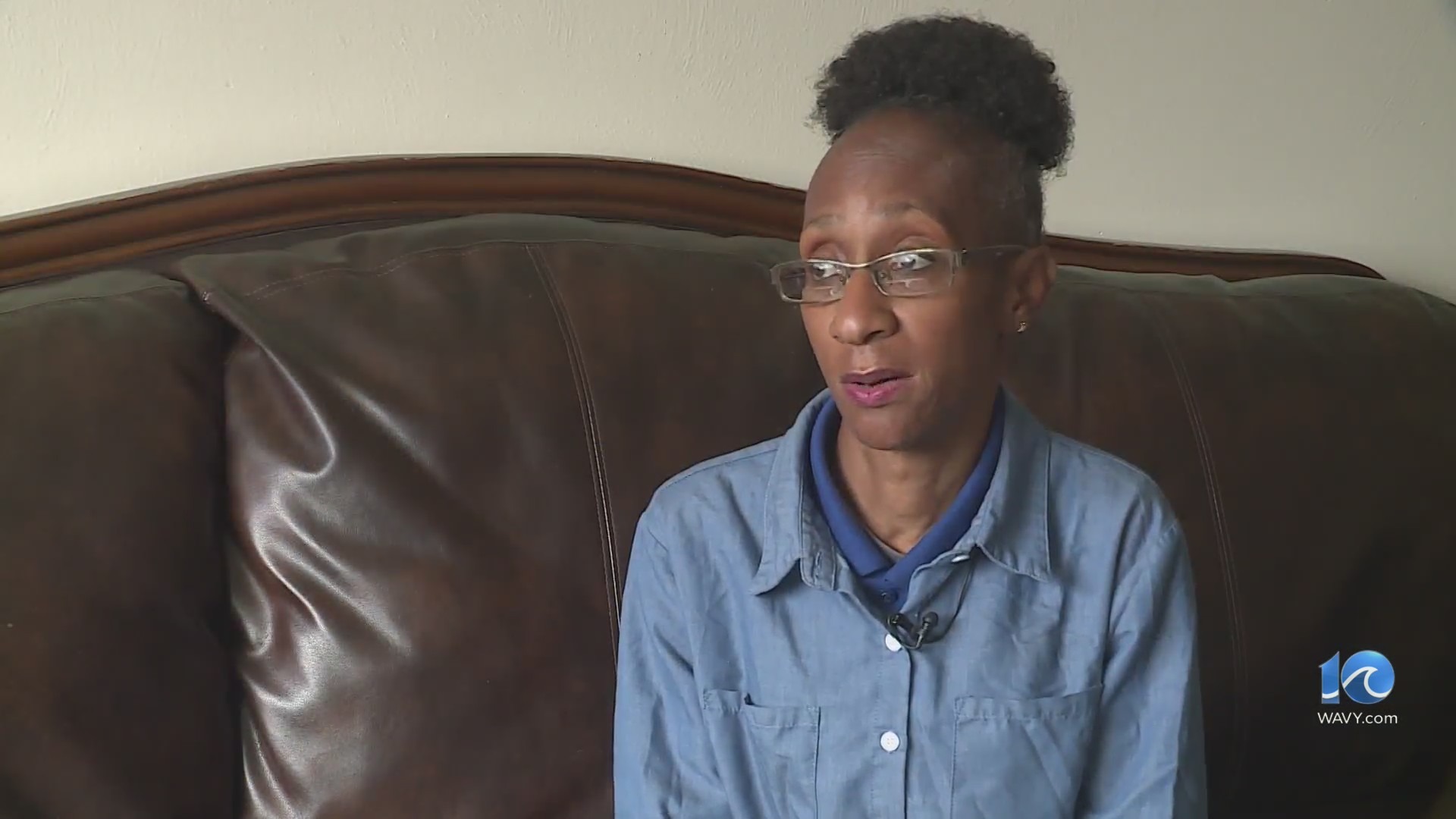
In 2020, Gov. Ralph Northam signed the Marcus-David Peters Act. The legislation was named after a Black, biology teacher who was fatally shot by Richmond Police in 2018 after he charged an officer in the midst of a behavioral health crisis.
The law creates the Marcus Alert System: a set of protocols for how teams of mental health providers and peer recovery specialists can reduce the role of law enforcement during crisis calls, including those involving substance abuse disorder and developmental disabilities.
“The aim is really to provide a mental health response to mental health emergencies and reduce negative outcomes involving use of force in law enforcement interactions,” said Mira Signer, Chief Deputy Commissioner for the Virginia Department of Behavioral Health and Developmental Services (DBHDS).
“A patchwork of resources has developed overtime and that has resulted in an over reliance on law enforcement,” Signer continued.
A detailed roadmap for implementing the Act was due on July 1 following a collaborative process between DBHSD, the Virginia Department of Criminal Justice Services (DCJS), and a Marcus Alert State Planning Stakeholder Group.
While the Act isn’t expected to be fully phased in until 2026, Signer said five areas are launching Marcus Alert Systems on December 1, 2021. Those include:
- Region 1: Orange, Madison, Culpeper, Fauquier and Rappahannock Counties
- Region 2: Prince William County
- Region 3: City of Bristol and Washington County, including the Towns of Abingdon, Damascus, and Glade Spring
- Region 4: City of Richmond
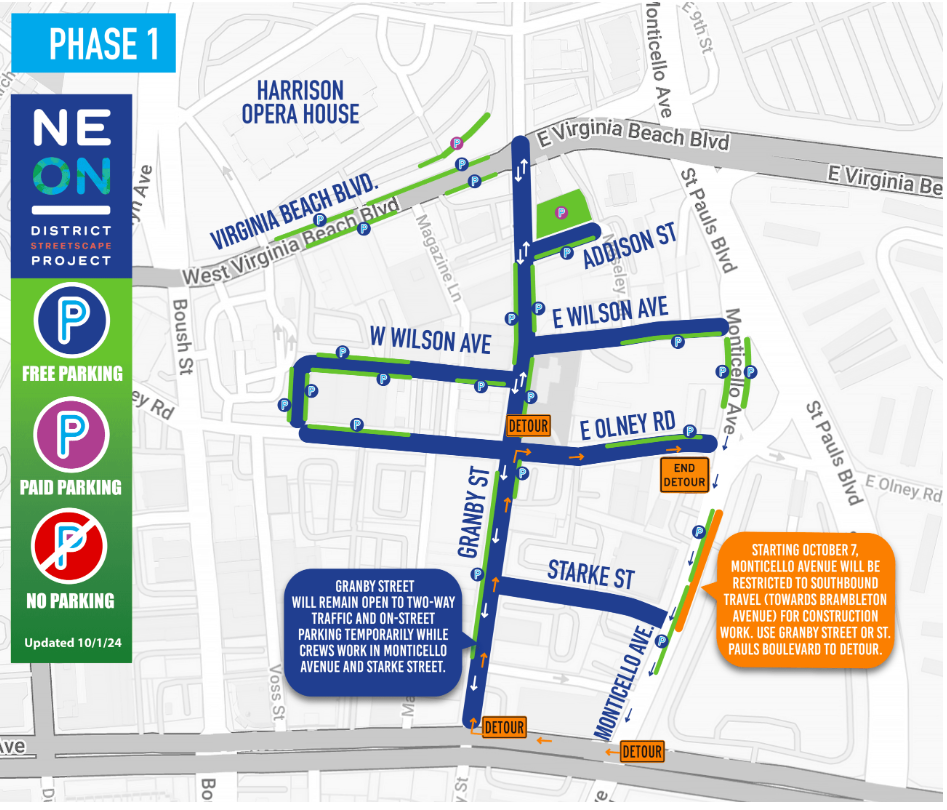
- Region 5: City of Virginia Beach
Signer said these five regions will be moving forward with the roll out of three main protocals. She said other localities will have to submit implementation plans by July 1, 2022.
First, she said local law enforcement agencies will be mandated to divert 911 calls with lower threat levels to regional call centers or the 9-8-8 suicide hotline.

Second, for situations where a police presence may be needed as back up, departments will need to enter into an agreement with a regional mental health mobile crisis response hub.
Lastly, Signer said officers must be governed by specialized requirements when they do respond to mental health-related calls that, among other things, aim to minimize the use of force.

As the state works to shape a new system, the Virginia Association of Chiefs of Police and the Virginia Association of Community Services Boards are questioning whether the General Assembly has allocated enough resources to carry out the policy shift to completion.
In an email, VACSB Executive Director Jennifer Faison said the Marcus Alert is “underfunded to meet the requirements of the model.”
“There are a multitude of challenges with the model that the General Assembly adopted,” Faison wrote.
Before the law passed, Faison said the state was already in the process of building a 24/7 mobile crisis response network through STEP VA that will support the Marcus Alert System.
To make comprehensive coverage a reality under this new model, Faison said a sustained increase in state funding is needed to implement protocals. She said that funding is also neccessary to recruit and retain behavioral health clinicians amid a severe workforce shortage.
Faison is also calling for a signficant investment of American Rescue Plan funds to provide one-time bonuses, tuition assistance and student loan debt repayment as incentives.
“We are absolutely concerned about the workforce in our system,” Faison wrote. “Community Services Boards are experiencing shortages in the workforce in all areas of their operations and workforce development continues to be a top priority.”
Asked about this concern, Signer said the state has put forth proposals that will increase the number of mobile teams and call center dispatch staff.
The state is also in the process of setting up integrated call centers to streamline and coordinate responses regionally. Currently, DBHDS says those access points are fragmented, which has created barriers to appropriate care.
However, the VACSB is concerned the December 2021 deadline laid out by the General Assembly to launch that service is rushed, considering the state is still trying to obtain a vendor.
“If the platform is not made available in a timely manner, it may well delay implementation of the protocols,” Faison said.
Asked if there is any chance of that happening, Signa said they state is on track: “We’re expecting it to be implemented by December 2021.”