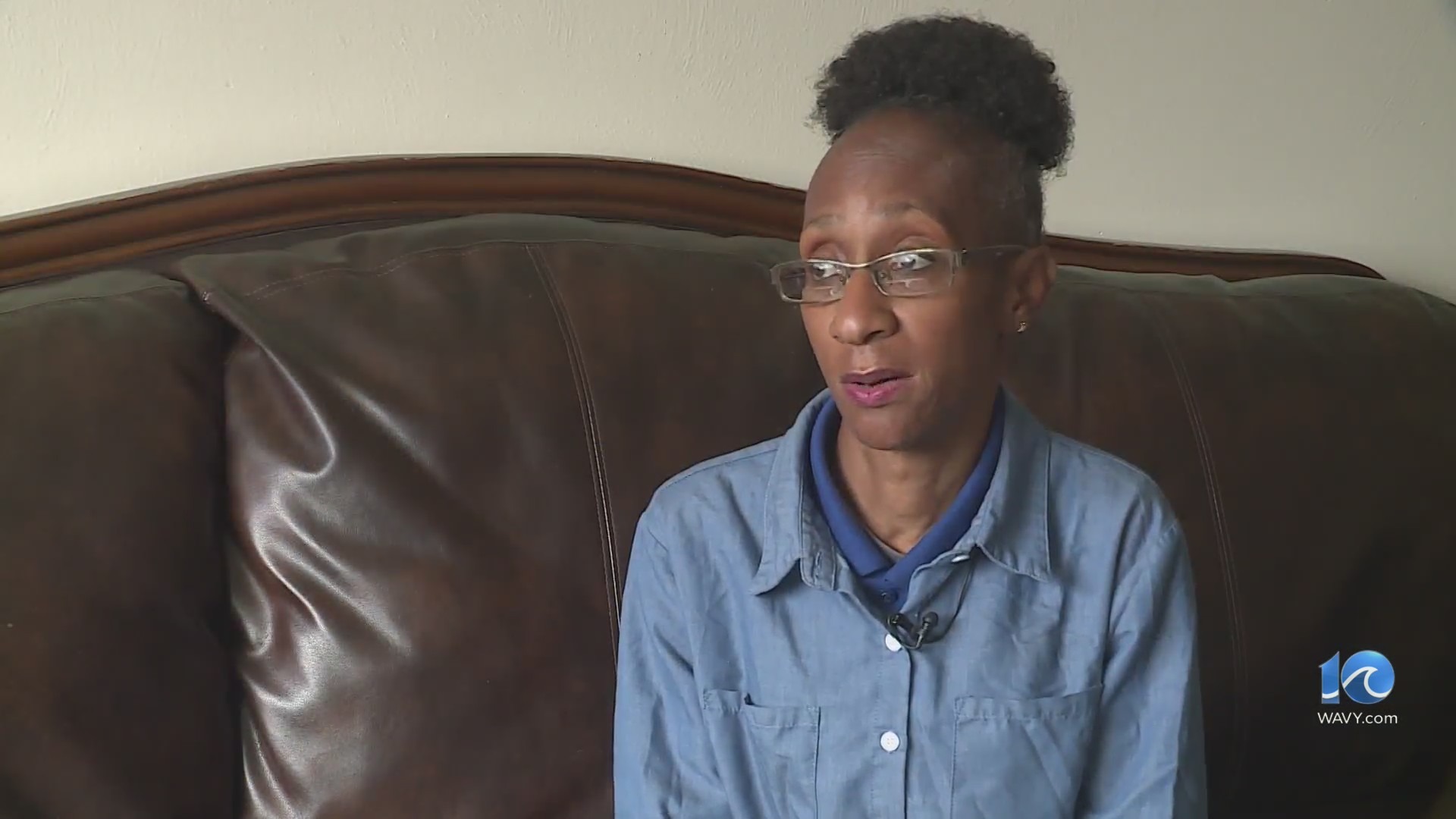
HAMPTON ROADS, Va. (WAVY) – In this Community Chat, WAVY Digital Desk Host Sarah Goode speaks with Dr. John Plemmons, a Sentara radiologist, about the new breast cancer screening guidelines. Watch the chat in the video player on this page.
According to the United States Preventive Services Task Force’s (USPSTF) new proposed guidelines, they now recommend women with average-risk get screened every other year for breast cancer starting at age 40. That’s 10 years earlier than the USPSTF’s 2016 guidelines that recommended women begin screening at age 50, with women in their 40s making individual decisions about screening. According to the USPSTF, the earlier screening could result in 19% more lives being saved.
The CDC says breast cancer is the second most common cancer among women in the United States. It is also the second leading cause of cancer deaths in women.
Screening for breast cancer
There are different methods of breast cancer screening.
According to Plemmons, mammography remains the most tested and proven tool available.
“Screening mammography may be good at picking up 95% of breast cancer in fatty breast tissue,” Plemmons said. “The sensitivity, or ability to pick up breast cancer in dense breast tissue is lower, about 65%. But 3D mammography has improved that significantly.”
Plemmons wants to make sure women know they need to come in before they have a lump, or any suspected symptoms.
“The purpose of a screening mammogram is to detect breast cancer before you feel anything,” Plemmons said. “(And) at the age of 40, get a screening mammogram. You will feel no symptoms. You’re the patient – we are trying to find that small breast cancer that has not shown itself in any way.”
Women should find out their individual risk to see if they need to be scanned earlier than 40. Plemmons suggests getting a risk assessment by age 25.
Health inequities and access to care
One issue the new USPSTF guidelines highlight is the need for more research on the health inequities people face related to breast cancer.
According to the USPSTF, Black women are 40% more likely to die from breast cancer than White women, and more likely to get deadlier cancers at a younger age.
Plemmons talked about the Find it Early Act as one way to combat inequities. The legislation is aimed at helping breast cancer detection and saving lives.
In a press release shared in December 2022, it states that “this bill would ensure all health insurance plans cover screening and diagnostic mammograms and breast ultrasounds and MRIs with no cost-sharing.”
On May 8, it was reintroduced to Congress.
Plemmons encourages the public to learn more about the act and contact their representatives about it.
One way Sentara is trying to help with access is through its 3D mammography van. The van offers care to those who may not have access. It also offers care to patients who are uninsured on a prorated basis. To book an appointment with Sentara’s 3D Mammography van, click here.
Differing guidelines across organizations
Not all organizations share the same recommendations.
The American College of Radiology has maintained a constant screening recommendation, that women get screened yearly starting at age 40.
In May, the American College of Radiology added new suggestions for high-risk women. One recent update states that “women with genetics-based increased risk (including BRCA1 carriers), those with a calculated lifetime risk of 20% or more and those exposed to chest radiation at a young age are recommended to have MRI surveillance starting at ages 25 to 30. These women should start annual mammography at ages 25 to 40, depending on type of risk.”
The public comment period for the USPSTF’s updated breast cancer screening guidelines ends June 5. Find out more here.
Watch the full Community Chat in the player on this page to hear more about early detection, testing, health inequities and more.