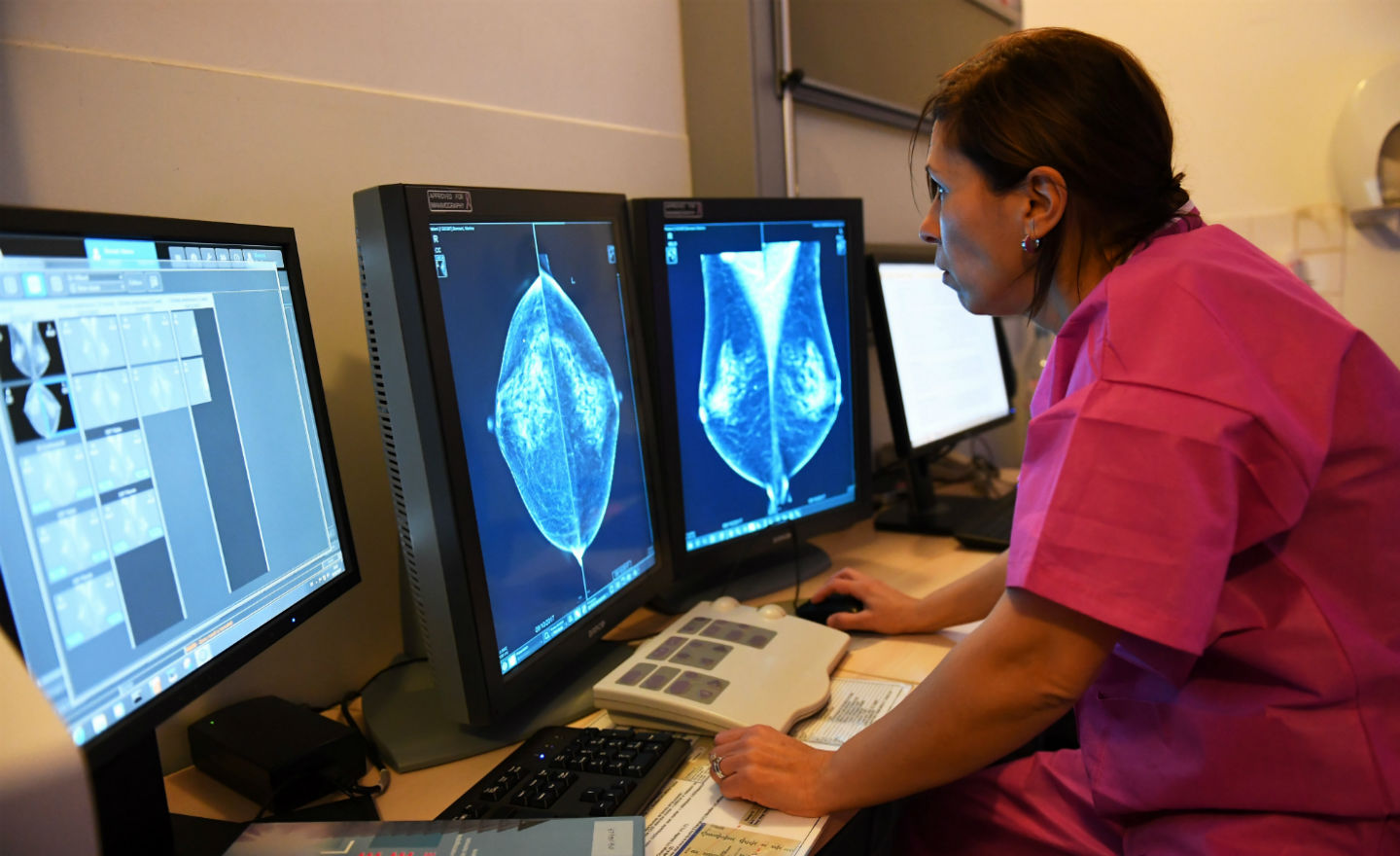
This article is part of a series marking Breast Cancer Awareness Month. Read Part 1 — Breast cancer rates are rising. But more women are surviving, too.
Breast cancer screening can save your life, so it’s important to familiarize yourself with guidance for your age group.
Recommendations on screening vary depending on your age and other risk factors — and have changed over the past year for women under 50.
The U.S. Preventive Services Task Force’s guidance is targeted at women who are at an average risk of breast cancer, which includes women with dense breasts and a family history of breast cancer.
Women who are high risk — due to certain genetic mutations, a history of radiation therapy, or previous biopsies or lesions — should consult their doctors for individualized screening plans.
Here’s an age-based guide to whether you should schedule your next screening, reach out to your doctor for more advice, or hold off for now.
Under 40
The task force does not have a recommendation for women under 40. That doesn’t mean their risk factor is zero, but the downside risks of mammograms must be weighed against the potential upside.
“There are benefits and also harms,” said Dr. Wanda Nicholson, the vice-chair of the U.S. Preventive Services Task Force. “As a task force, we look at the balance of those benefits and harms.”
These harms include false positive screenings, unnecessary biopsies, and overdiagnosis, which can all lead to financial, physical, and psychological strain.
Still, screening may be recommended for some women under 40 with certain risk factors, such as family history, radiation exposure, breast density or gene mutations.
Talk to your doctor about the personalized screening plan that is right for you.
40-50
The U.S. Preventive Services Task Force changed its recommendations for women between 40 and 50 this year.
All women aged 40-74 are now encouraged to start getting screened every other year.
Previously, the recommendation was for women aged 40-50 to make an individual decision with their doctors about screening.
“We’re recommending that all women, regardless of background, demographic, background, undergo screening beginning at age 40 and continue every other year.”
The recommendation was changed due to “new and inclusive” data, including rising incidence rates in the age group every year since 2016, Nicholson added.
The new recommendation has the potential to save up to 1.3 more lives for every 1,000 women over a lifetime of screening, according to statistical models used by the task force.
50-75
The recommendation for women between 50-75 has stayed the same — be sure to get biennial screenings.
“The importance is that getting screened for breast cancer can save your life,” Nicholson said.
75 and older
The task force is still collecting data as to the best recommendation for women over 75. These women should consult their doctors for an individualized screening plan.
Studies have shown that the risk of overdiagnosis and overtreatment is particularly high for women over 75 and continues increasing along with age.
Overdiagnosis is not the same as false positives; it refers to detecting cancers that develop too slowly to cause health problems in a patient’s lifetime.
“The suggestion that screening may not be helpful is tricky,” said Dr. Ilana Richman of Yale School of Medicine, who led a recent study on the issue.
“We don’t want our patients to think that we’re giving up on them, when what we’re really after is just the opposite — focusing on care that improves quality of life by avoiding tests that are unlikely to be beneficial.”
Non-cisgender
The Task Force’s recommendations apply to all individuals who were assigned female at birth, including transgender men and nonbinary people. That is because the benefit estimates are driven by sex, rather than gender identity.
More information
Read more about the U.S. Preventive Services Task Force’s draft recommendation on breast cancer screening.
And here is a guide to assessing your risk factor from the Breast Cancer Research Foundation.
Updated: Oct. 31 at 1:03 p.m.