HAMPTON, Va. (WAVY) – Beginning August 5, a new acting director of the Hampton VA Medical Center will have to right a ship that is reeling over findings of substandard surgical practices.
Walter Dannenberg comes to Hampton from Long Beach, California, where he’s directed the VAMC for the past seven years. Dannenberg has also served at VA centers in Arkansas and Washington State. He has to turn around Hampton after the Office of the Inspector General’s highly critical report that focused on surgery, and specifically the assistant chief of surgery.
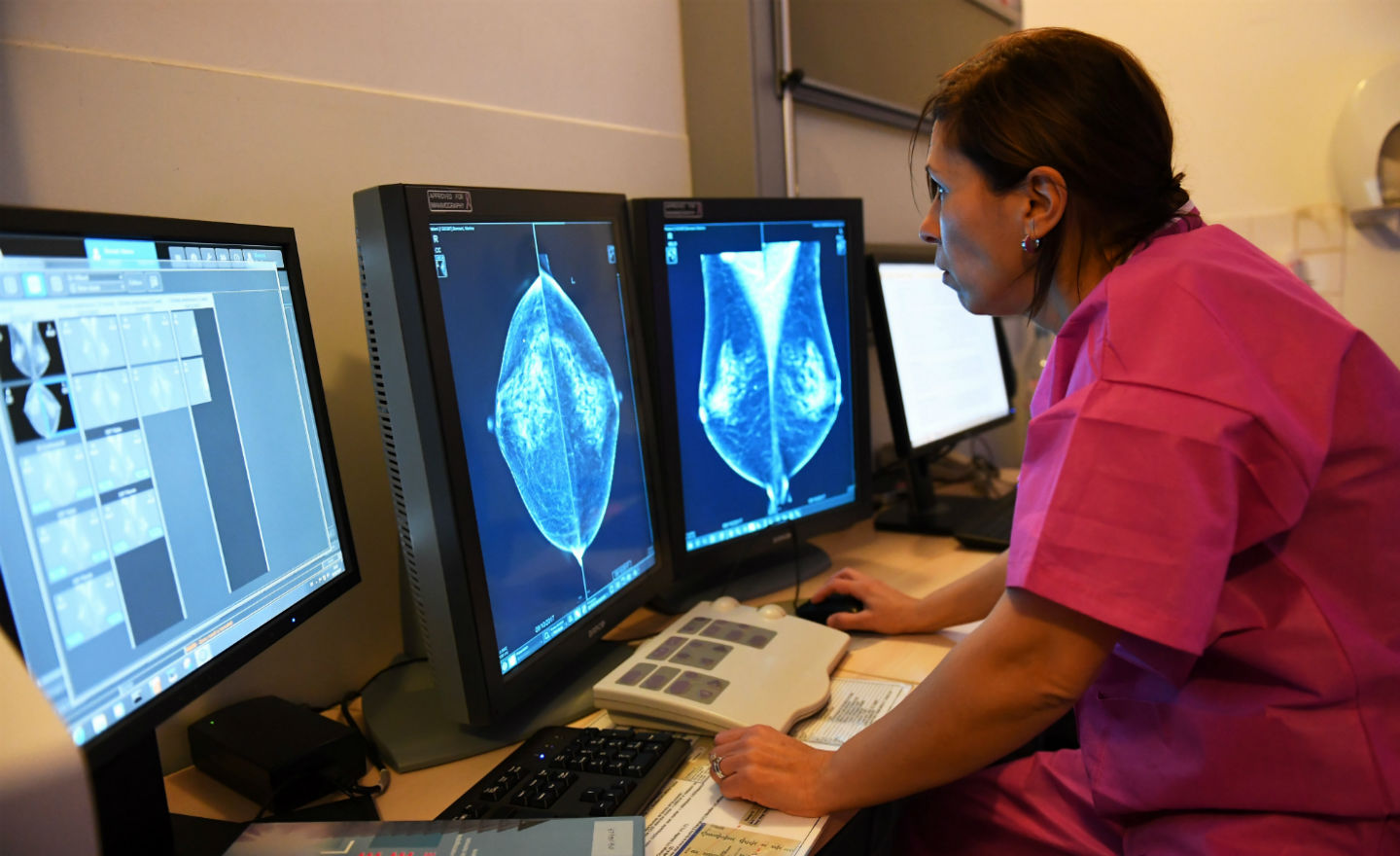
The report from the Inspector General cites several different areas where the surgery department at the Hampton VA Medical Center failed, including substandard care, the competency of the assistant chief of surgery, the medical center’s failure to inform patients of potential compensation from adverse surgical outcomes, and its failure to report the surgeon to state regulators.
The report focuses on six cases involving the assistant chief of surgery that were found to have substandard care, including a robotic-assisted procedure following a diagnosis of rectal cancer; a Crohn’s patient’s procedure; a colon cancer patient whose liver was lacerated during surgery; a diverticulitis patient whose surgery led to infection; another diverticulitis patient whose liver and gallbladder were injured during surgery; and a rectal cancer patient who also had COPD and was under general anesthesia for too long.
The OIG looked into whether the assistant chief of surgery was “unsafe,” but found her to be competent, and added that two general surgeons operate on the more complex surgical procedures.
A source told 10 On Your Side the woman identified only by the title of assistant chief of surgery in the report, and not by name, has been gone from the medical center for several months.
The OIG report also cited Hampton for failing to inform patients and their families about compensation options – if their surgeries result in what they call “adverse outcomes.”
Medical centers are required to tell them they can seek compensation either from the Veterans Benefits Administration and under the Federal Tort Claims Act.
And the report says the Hampton VA failed to report the assistant chief of surgery to the Virginia Licensing Board, which it must do when there’s evidence the provider failed to meet generally accepted standards.
The Department of Veterans Affairs issued this statement to WAVY in response to the OIG report, from Press Secretary Terrence Hayes:
“At VA, our mission is to ensure Veterans get the world-class health care they deserve from caring, qualified professionals – and we will never settle for anything less. We take allegations of oversight and misconduct seriously and have strengthened our policies and procedures to ensure consistent, high-quality care from licensed professionals. VA uses rigorous credentialing, privileging processes, and administrative reviews to maintain care quality and integrity. Our mission is to deliver world-class health care to Veterans through skilled and compassionate professionals, and we are committed to upholding these standards.
VA values the Office of the Inspector General (OIG) review and fully supports its findings. We are taking urgent action to address the OIG’s recommendations, and we plan to fully implement all recommendations by December 2024. These steps include:
Leadership’s Actions to Date:
- Established a bi-weekly multidisciplinary team to address open OIG recommendations, targeting year-end completion.
- Conducted multiple reviews, resulting in the creation of a reporting tool to track clinical care metrics, suspensions, privilege changes, state board reports, and ongoing evaluations.
- Initiated monthly patient risk meetings in Surgery Services to address potential safety concerns, reduce patient cancelation and mitigate risk.
- Initiated ongoing quality and reporting training for surgical staff, enhancing their understanding of the safety reporting tool.
Surgery Department Stats:
- Received a three-year reaccreditation from The Joint Commission’s Gold Seal of Approval in January 2024.
- Earned Intersocietal Accreditation Commission (IAC) Accreditation for vascular testing in April 2024, one of 13 out of 172 VA facilities.
- Performed 1,761 cases in FY23 and FY24, with a Veteran Trust Score of 86.7%.
- Reported zero critical incidents in FY23 and FY24.
- Achieved a surgical site infection rate post-discharge significantly lower than the national average, nearing zero.
Best Practices Noted During the VISN 6 Surgery Review:
- The Surgery department maintains low morbidity and mortality rates post-surgery, reflecting quality patient care as per National Surgical Office metrics.
- The Operating Room’s Morning Huddle, led by the OR Nurse Manager, effectively identifies and addresses daily case barriers.
- The Anesthesia Section’s pre-operative clinic risk-stratifies patients and schedules additional consultations as needed, reducing same-day surgery cancellations due to incomplete assessments.
“While progress has been achieved, continuous improvement is essential to maintain the highest quality care,” the VA said. “We value oversight and collaboration with the OIG, our staff, stakeholders, and VA officials, as it strengthens our mission to honor and care for Veterans.”